We try to educate others about our everyday life as much as possible, especially when it comes to unique medical things that we ourselves knew nothing about six months ago.
That is the goal of this post: to show what it is like to feed Tori through a G-Tube and how that affects our lives.
Tori first received a feeding tube on February 6, 2015 (NG Tube, which goes through the nose to the stomach). She had stopped nursing well and wouldn’t take a bottle. This was a symptom of Krabbe but we didn’t know that at the time.

Hershey Medical Center provided us with adorable stickers for the tube because, as the nurses said, if she was going to have a tube it would at least look cute 😉
She had her G-Tube/Nissen surgery on March 23rd at Hershey Med and I was afraid to take care of it. Other Krabbe parents had said it would make life so much easier but I didn’t believe it. This was much scarier than a tube through her nose – this was a portal directly into her stomach!
But, they were right. The G-Tube makes feedings fairly simple, and the Nissen has greatly decreased her vomiting (a Krabbe problem that she had from birth).
Another plus was that we were able to see her beautiful face again!
So, what do feedings look like?
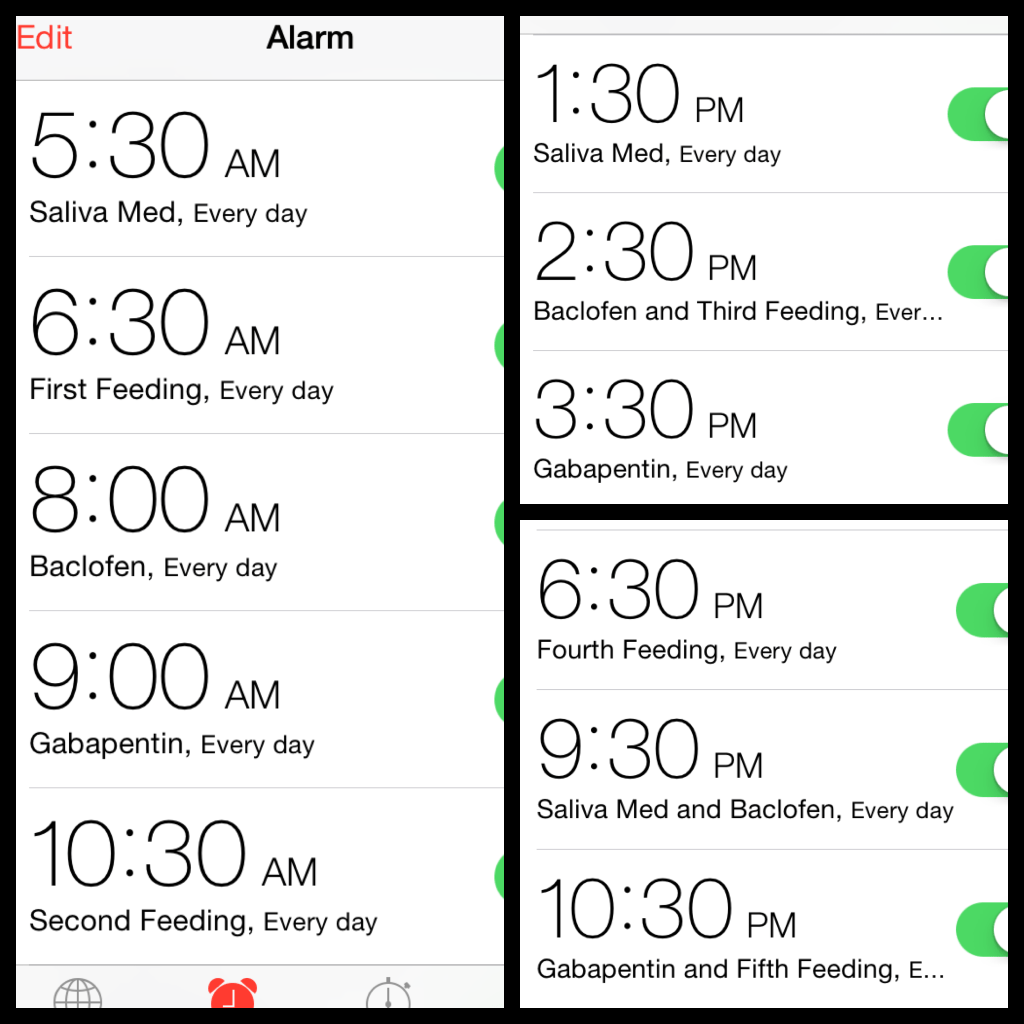
Well, to start, here is what our schedule looks like currently:
Having a strict schedule helps us ensure that meds are given at the proper increments (some have very precise rules about timing), and it also helps us plan excursions because we easily know what she will need while we are out.
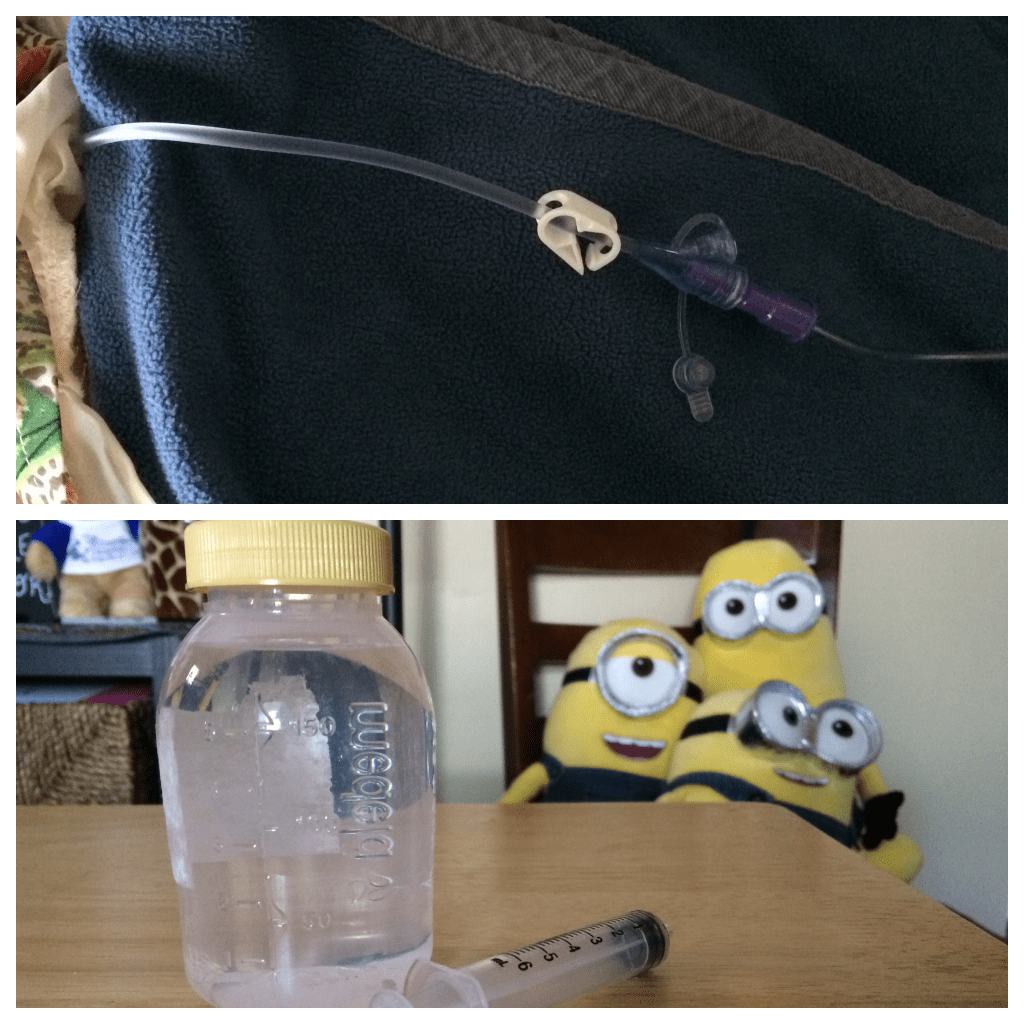
There are many pieces of equipment and many supplies that are always on hand and they are delivered to our home monthly: feeding bags, G-Tube extensions, syringes, etc.
On the left is the G-Tube, also known as a MIC-key Button. We replace it every few months at home. We use the pads on the right instead of gauze to absorb any residue that comes out of the tract. The pads are changed 1-2 times a day.
Below is the pump and pole that we use at home. Her adaptive stroller also has a pole, and we have a portable IV pole for traveling. This works far better for us than the backpack that came with the pump because we always had issues with keeping the bag above the pump to avoid air getting into the tube.
The pump regulates the speed of the feed to ensure that she can tolerate it. She currently eats 125mL over an hour, five times a day. This is slower than it was even a month ago, and it will slow down further as the disease progresses.
We use three feeding bags a day, switching them every other feed.
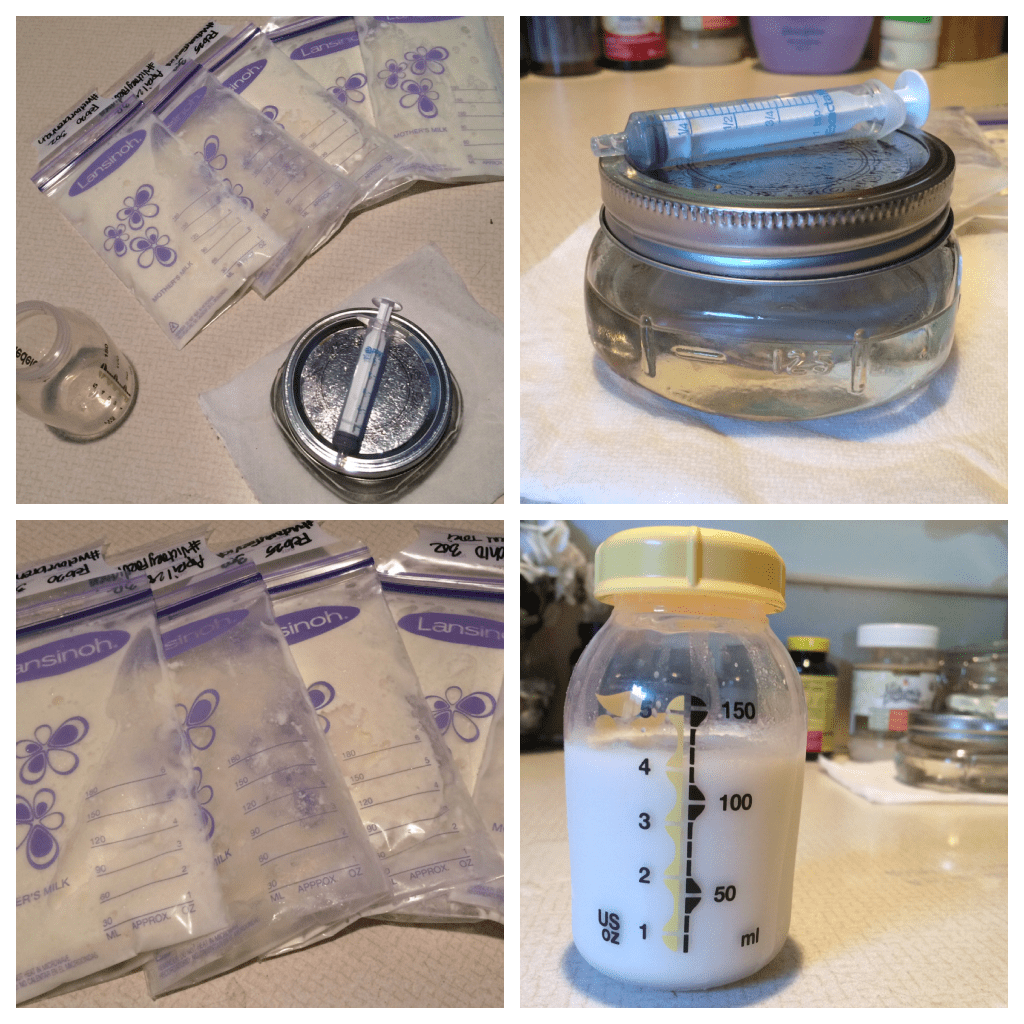
Tori is still on breastmilk thanks to generous friends who donate their pumped milk to us for free. Some have even shipped it across the country for us!
The milk is frozen in bags in one of our deep freezers (we had to buy one just to hold all of the milk we receive!). If I am on top of it, I try to defrost the milk for the next 24 hours by letting it sit on the counter for about an hour – that way it is still really cold and can safely go in the fridge. I then pour the proper amount into five bottles and add the MCT oil to it (MCT oil is a coconut-based oil that is easily absorbed into the body. Tori has difficulty processing fat of any kind so this is helping her gain weight).
The bottles are then placed back in the fridge until it is time for a feeding. We have a breastmilk warmer that is fantastic and it ensures that the milk is warmed evenly and safely.
The milk is then poured into the feeding bag, the pump is primed (pushes milk all the way through the tubing to ensure that air isn’t pushed into Tori’s belly), and we begin the feed.
One of the pros of tube feeding is that she doesn’t have to be awake.

The milk goes through the extension into the MIC-key button and into Tori’s stomach. After each med or each feed, we flush the tube with 5mL of distilled or bottled water.
She has gained three pounds since her surgery four months ago! This process is complicated but it has become part of our daily life and we rarely think about what a pain it can be (except now, as I write all of this out, haha).
Her doctors have encouraged us to still allow her to taste small amounts of things so that she isn’t deprived of the joy of taste. We often forget simply because of the stress of everything we have to do each day for her, but when we do remember she really appreciates it!
I miss the ease and convenience of breastfeeding, but knowing that she is safely consuming her calories without risk of aspiration makes all of this worth it.




I wish and pray for your strength and resolve to continue this journey with your beautiful child………you are amazing people, filled with the love of Jesus Christ. In Him we do have hope……….
LikeLike